Osteoporosis is a continual disease that negatively impacts bone density and strength, escalating the potential for bone fractures and diminishing the quality of life.

Bones are perpetually undergoing a process of degradation and reconstruction, a cycle known as bone remodeling, which demands sufficient levels of specific nutrients.
Therefore, it is reasonable to question if particular dietary supplements, when coupled with a nutritious diet, can assist in forestalling and controlling this disease.
This article scrutinizes the scientific evidence related to 11 supplements, their role in the prevention and management of osteoporosis, and any possible disadvantages.
In this article
1. Vitamin D
Vitamin D is essential for bone health. It plays a key role in calcium absorption and helps regulate bone turnover.
Given the limited number of food sources of this vitamin, which includes fatty fish and fortified dairy products and cereals, most people obtain vitamin D through sunlight exposure.
However, getting adequate amounts of vitamin D through sunlight exposure can be difficult during the winter and for those who spend the majority of their time indoors.
Furthermore, people who live far north or south of the equator are at an even greater risk of vitamin D deficiency due to limited sun exposure for up to 2–5 months per year.
One study including 400 older adults found that people with osteoporosis were more likely to be deficient in vitamin D. Of those deficient in vitamin D, daily intake of a vitamin D supplement was also linked to a lower incidence of osteoporosis over 8 weeks.
That said, while vitamin D supplements may be beneficial for people with vitamin D deficiency, research has not observed benefits of vitamin D supplements once blood levels are at or above sufficiency levels.
The current reference daily intake for vitamin D is 600 IU for children and adults ages 1–70 and 800 IU for pregnant or breastfeeding adults and those 71 years or older.
To reduce the risk of bone fractures and ensure sufficient blood levels, research suggests that a dose of 400–800 IU of vitamin D per day may be sufficient.

Interestingly, one study including 311 healthy adults found high doses of 4,000 and 10,000 IU of vitamin D per day resulted in a greater loss of bone mass density over 3 years than taking a smaller 400 IU daily dose.
Still, while research suggests smaller doses may be better in the long term for bone density, higher doses may be needed temporarily in more severe vitamin D deficiency cases.
Given that it’s estimated that 50% of the population has low levels of vitamin D, it’s worth talking to a healthcare provider if you’re concerned about not getting adequate vitamin D throughout the year.
Summary: Vitamin D is essential for bone health. Vitamin D supplements may benefit people who are deficient in this vitamin.
2. Magnesium
Magnesium is an essential mineral that’s involved in over 300 reactions in your body. It’s also important for bone health, with approximately 60% of this mineral being found in bone tissue.
The recommended daily intake for magnesium is 310–320 mg per day for people ages 19–30 years and 400–420 mg per day for people ages 31 and older. Needs are also slightly elevated during pregnancy and breastfeeding.
One study in 51 postmenopausal women found that 40% of women with osteoporosis or low bone density had low circulating magnesium levels.
Additionally, several studies in adults have found that individuals who consume higher amounts of magnesium through their diet or supplements have better bone mass density than those consuming low amounts.
Suggested read: Calcium Supplements: Should You Take Them? Benefits & Risks
While adequate magnesium intake has been associated with bone density benefits, research is mixed on whether this benefit translates into a reduced risk of bone fractures.
As more research is needed on the role and optimal dose of magnesium supplements on the risk of osteoporosis and bone fractures, it’s best to focus on consuming a diet rich in magnesium-containing foods, such as nuts, seeds, whole grains, and legumes.
If you’re concerned about meeting your magnesium requirements through diet alone, you should speak with your healthcare provider for personalized recommendations on magnesium supplements.
Summary: Adequate magnesium intake is important for overall bone health and bone density. Yet, more research is needed on magnesium supplements’ role in preventing bone fractures.
3. Boron
Boron is a trace element that has been found to play a critical role in bone growth and maintenance. It affects the use of other nutrients needed for bone health, including calcium, magnesium, and vitamin D.
Currently, there’s no established recommended daily intake for boron. Still, based on current research, it’s thought that 1–3 mg of boron per day may be beneficial.
An older study in postmenopausal women found taking 3 mg of boron per day significantly reduced the excretion of calcium and magnesium in the kidneys.
Additionally, one study in rats with osteoporosis found boron supplementation significantly reduced bone loss. However, research confirming this effect in humans is currently lacking.
As dried plums are one of the best dietary sources of boron, limited research has examined the relationship between dried plum intake and bone density in humans.
For example, one study in 48 postmenopausal women with low bone density found that consuming 50–100 grams of dried plums per day resulted in significant bone density improvements over 6 months.
Suggested read: How Much Vitamin D Should You Take for Optimal Health?
While the exact mechanism isn’t fully understood, it’s thought that the boron content in the dried plums may partially explain why these fruits have been shown to have benefits for bone health.
Boron is not regularly found in multivitamin supplements. As a result, it may be easier to consume it through foods, including prunes, raisins, and dried apricots.
Summary: Boron is a trace element involved in bone growth and maintenance. While more research is needed, it has been suggested that 1–3 mg of boron per day may support bone health.
4. Vitamin K
Vitamin K plays an important role in maintaining bone strength and preventing bone breakdown. Low levels of vitamin K have been associated with an increased risk of bone fractures and low bone density.
There’s currently no defined recommended daily intake for vitamin K. Instead, the adequate intake for adults over 18 is set at 90 mcg per day for women and 120 mcg per day for men.
While research suggests a protective effect of adequate vitamin K intake on bone density and fractures, it’s inconclusive whether vitamin K supplements protect bone health.
Given that more research is needed on the role of vitamin K supplements on osteoporosis and related fractures, it may be best to consume foods rich in vitamin K, such as leafy greens, broccoli, and Brussels sprouts.
It’s important to note that vitamin K can interfere with several medications, including blood thinners like warfarin. As a result, it’s important to talk with your healthcare provider before taking vitamin K supplements.
Summary: Low levels of vitamin K have been associated with low bone density and risk of fractures. More research is needed to determine whether taking vitamin K supplements may help prevent bone loss and fractures.
5. Soy isoflavones
Isoflavones are a class of antioxidants often referred to as phytoestrogens. They have a structure similar to that of the hormone estrogen and can attach to and activate estrogen receptors in your body.
Suggested read: 10 Natural Ways to Build Healthy Bones
During menopause, estrogen levels in the body decline. This drop in estrogen can lead to the bone being broken down faster than it can be formed, resulting in an increased risk of osteoporosis.
Research suggests that soy isoflavones may help combat this loss of calcium from the bone and reduce the rate of bone turnover.
One review of 19 studies in postmenopausal women found soy isoflavone intake through supplements significantly increased bone mineral density by 54% and reduced bone resorption marker by 23%, compared with their baseline values.
Similarly, another review of 52 studies showed significant bone density improvements with soy isoflavone supplementation in studies lasting for at least a year.
While promising, it’s important to note the large variability in the dosage and supplement form used between studies. As a result, the suggested dosage based on current research is quite broad.
It’s currently thought that 40–110 mg of soy isoflavones per day for at least a year may help combat bone loss and protect against osteoporosis.
Keep in mind that more research is needed on differences in dosage requirements across various age groups and ethnicities, the duration of supplementation, and the form used.
Summary: Soy isoflavone supplements have been shown to improve bone density and reduce bone turnover in postmenopausal women. More research is needed to determine the optimal dosage and supplement form.
6. Calcium
Calcium is a major component of bone tissue and essential for bone strength and structure. Approximately 99% of your body’s calcium is stored in your skeleton.
The current recommended daily intake for calcium ranges from 700–1200 mg per day, with increased needs during certain life stages, including childhood and adolescence, pregnancy and lactation, women over the age of 50, and all adults 70 years or older.
While adequate calcium intake throughout your life is important for bone health, research on the potential benefits of taking calcium supplements for the prevention and management of osteoporosis is mixed.

One review of 8 studies found calcium plus vitamin D supplements were linked to a 15–30% reduced risk of fractures in both community-dwelling and institutionalized middle-aged and older adults.
However, another review of 33 studies found that calcium supplements — either on their own or in combination with vitamin D — weren’t associated with a reduced risk of fractures in older adults living at home, compared with a placebo.
Similarly, a review of 59 studies found that increasing calcium intake through either supplements or food sources resulted in small but not clinically meaningful improvements in bone mass density.
Overall, while calcium supplements may be appropriate for individuals who are at an increased risk of deficiency, there’s currently insufficient evidence to recommend calcium supplements to prevent or manage osteoporosis in the general population.
Potential concerns with calcium supplements
There are some concerns about taking large doses of calcium via supplements.
For example, calcium supplements have been associated with symptoms like constipation, kidney stones, and other digestive issues. There are also some concerns that they may be harmful for heart health.
One review found an increased risk of heart attacks in those taking calcium supplements. That said, other studies have not shown a link between calcium supplements and negative outcomes for heart health.
As dietary intake of calcium has not been linked to these side effects, it’s best to focus on meeting your calcium needs through your diet and discussing the potential need for supplements with your healthcare provider.
Summary: While there are certain situations in which calcium supplements may be indicated, the current research doesn’t support the widespread use of calcium supplements to prevent or manage osteoporosis.
7–11. Other supplements
Several trace minerals and elements play essential roles in bone health and may support bone density and reduce the risk of fractures. They include:
Suggested read: 9 Important Health Benefits of Vitamin B12
- Zinc. Zinc is important for bone growth; higher zinc levels have been linked to better bone density scores. Additionally, low zinc levels have been found in women with osteoporosis and low bone density.
- Selenium. Observational studies have shown a link between higher selenium intake and bone density and osteoporosis risk benefits. Yet, research on the effectiveness of selenium supplements is lacking.
- Copper. One study found a link between low copper levels and lower bone density measurements. However, research on copper for osteoporosis prevention and management is overall limited and inconsistent.
- Manganese. Observational studies have associated adequate manganese levels with benefits for bone density. Further research is needed to examine the role of manganese supplements in bone health.
- Silicon. In animal studies, silicon supplements have been shown to increase bone density and reduce fragility. However, research in humans is limited to just a few older studies.
While it’s important to get adequate amounts of these minerals in your diet, more research is needed on whether these supplements can help protect against osteoporosis and related fracture risk.
Several herbal supplements are also used in alternative medicine to help treat osteoporosis. However, the effectiveness of these supplements in humans is not currently supported by research.
Summary: Overall, more research is needed to determine whether taking certain trace minerals and elements as supplements help prevent or manage osteoporosis.
Who may benefit from supplements
It’s generally recommended to meet your nutrient needs for bone health via a healthy, balanced diet. However, some individuals may struggle to do so.
In particular, vitamin D can be difficult to obtain through diet alone.
While it can be synthesized from sunlight during certain times of the year, vitamin D supplements may be indicated for people with limited exposure to sunlight due to their location, lifestyle, or the time of year.
Additionally, due to naturally occurring changes in the skin with age, older adults may be less effective at synthesizing vitamin D.
Suggested read: How Much Vitamin B12 Is Too Much? Safe Dosage & Risks
Other compounds important for bone health, including magnesium, calcium, vitamin K, and soy isoflavones, are widely available in foods.
However, some instances in which supplements for these nutrients may be indicated include:
- restricted access to food
- a chronically poor appetite
- conditions causing nutrient malabsorption
- pregnancy and breastfeeding
- bariatric surgery, such as gastric bypass
- some vegan or vegetarian diets
- restrictive diets
It’s important to keep in mind that many supplements may have unintended side effects and interact with certain medications.
Overall, if you’re concerned about consuming enough nutrients to support bone health, it’s important to talk with your healthcare provider for personalized recommendations before taking supplements.
Summary: Diet is the preferred way to obtain essential nutrients for bone health. However, there are certain situations in which supplements may be indicated. Always talk with a healthcare provider before adding any supplements to your regimen.
Summary
Nutrition alone cannot cure or fully prevent osteoporosis. However, it can play a key role in the management and prevention of the disease.
While certain nutrients are important for bone health, including vitamin D, magnesium, boron, and vitamin K, more research is needed on the effectiveness of consuming them as supplements.
If you’re concerned about getting adequate nutrients for bone health through your diet alone, it’s best to talk with a trusted healthcare provider for specific recommendations before taking any supplements.
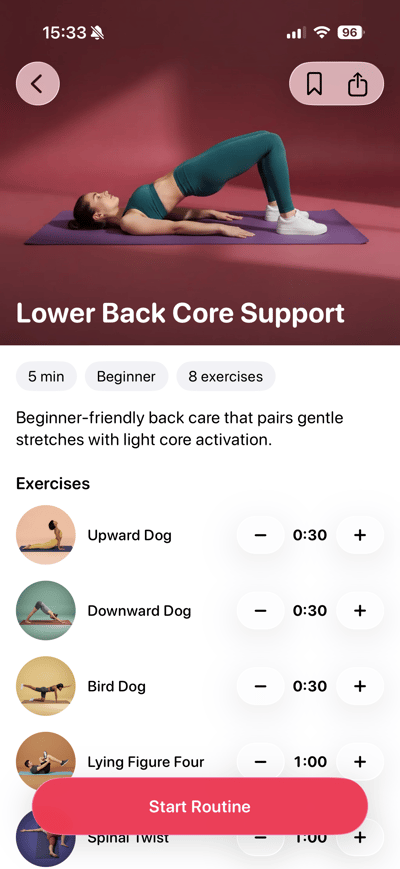
 Lose weight
Lose weight
 Gain muscles
Gain muscles
 Eat healthy
Eat healthy
 Explore new cuisines
Explore new cuisines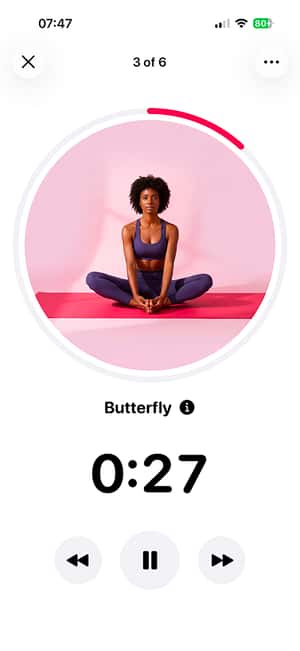
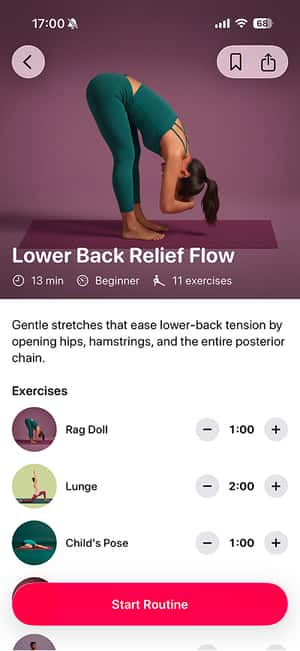
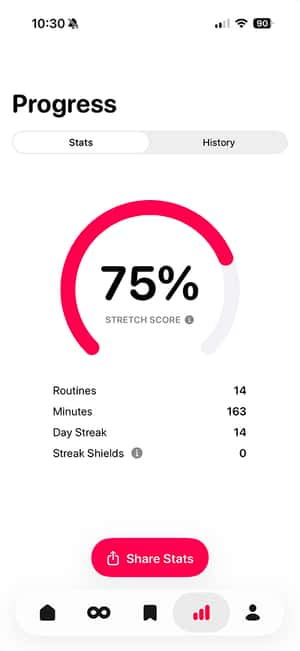
 Available on the App Store
Available on the App Store