Hashimoto’s thyroiditis — sometimes called Hashimoto’s disease or Hashimoto’s — is one of the most common thyroid disorders in the United States and other developed countries.

Even when treated with medication, its symptoms may significantly affect quality of life.
Research shows that diet, lifestyle modifications, and standard medication may drastically improve symptoms. Every person with Hashimoto’s thyroiditis responds differently to treatment, which is why an individualized approach to this condition is so important.
This article explains the diet and lifestyle modifications most likely to benefit those with Hashimoto’s thyroiditis.
In this article
Hashimoto’s thyroiditis overview
Hashimoto’s thyroiditis is an autoimmune condition that gradually destroys thyroid tissue via lymphocytes, which are white blood cells that are part of your immune system.
The thyroid is a butterfly-shaped endocrine gland at the base of your neck. It secretes hormones that affect nearly every organ system, including your heart, lungs, skeleton, and digestive and central nervous systems. It also controls metabolism and growth.
The main hormones secreted by the thyroid are thyroxine (T4) and triiodothyronine (T3).
Eventually, damage to this gland leads to insufficient thyroid hormone production.
Summary: Hashimoto’s thyroiditis is an autoimmune condition that affects your thyroid, eventually causing inadequate hormone production.
How diet and lifestyle affect Hashimoto’s
Diet and lifestyle play vital roles in managing Hashimoto’s, as numerous individuals find their symptoms persist even with medication. Plus, many people who exhibit symptoms aren’t given medication unless they have altered hormone levels.
Moreover, research suggests that inflammation may be a driving factor behind the wide range of Hashimoto’s symptoms. Inflammation is often tied to diet.
Diet and lifestyle modifications are key to reducing your risk of other ailments, as people with Hashimoto’s thyroiditis have a higher risk of developing autoimmune conditions, high cholesterol, obesity, and diabetes.

Research shows that cutting out certain foods, taking supplements, and making lifestyle changes may significantly improve symptoms and quality of life.
These changes may help reduce inflammation, slow or prevent thyroid damage caused by elevated thyroid antibodies, and manage body weight, blood sugar, and cholesterol levels.
Summary: Diet and lifestyle changes may significantly decrease antibody levels, improve thyroid function, and reduce symptoms caused by Hashimoto’s thyroiditis.
Evidence-based dietary tips
Here are some evidence-based dietary tips to help treat Hashimoto’s thyroiditis.
Gluten- and grain-free diets
Many studies indicate that those with Hashimoto’s are more likely to have celiac disease than the general population. As such, experts recommend that everyone diagnosed with Hashimoto’s be screened for celiac disease.
Moreover, some evidence suggests that gluten- and grain-free diets may benefit people with Hashimoto’s thyroiditis.
In a 6-month study of 34 women with Hashimoto’s thyroiditis, a gluten-free diet reduced thyroid antibody levels while improving thyroid function and vitamin D levels, compared with a control group.
Many other studies note that people with Hashimoto’s thyroiditis — or autoimmune diseases in general — likely benefit from a gluten-free diet even if they don’t have celiac disease.
You avoid all wheat, barley, and rye products when following a gluten-free diet. For example, most pasta, bread, and soy sauces contain gluten — though gluten-free alternatives exist.
Suggested read: Supplements and Thyroid Health: What to Know
A grain-free diet is more restrictive than a gluten-free diet, as it bans all grains. Although this dietary change may also offer benefits, research is limited.
The Autoimmune Protocol diet
The Autoimmune Protocol (AIP) diet is designed for people with autoimmune diseases. It removes potentially harmful foods like grains, dairy, nightshades, added sugar, coffee, legumes, eggs, alcohol, nuts, seeds, refined sugars, oils, and food additives.
In a 10-week study of 16 women with Hashimoto’s thyroiditis, the AIP diet significantly improved quality-of-life scores. It significantly decreased levels of the inflammatory marker C-reactive protein (CRP).
Although these results are promising, larger longer-duration studies are needed.
Remember that the AIP diet is a phased elimination diet and should be prescribed and monitored by an experienced healthcare professional.
Consider avoiding dairy
Lactose intolerance is very common among people with Hashimoto’s thyroiditis.
In a study of 83 women with Hashimoto’s thyroiditis, 75.9% were diagnosed with lactose intolerance.
If you suspect lactose intolerance, cutting out dairy may aid digestive issues, thyroid function, and medication absorption. Remember that this strategy may not work for everyone, as some people with Hashimoto’s tolerate dairy perfectly.
Focus on anti-inflammatory foods
Inflammation may be a driving force behind Hashimoto’s thyroiditis. As such, an anti-inflammatory diet rich in fruits and vegetables may significantly improve symptoms.
A study of 218 women with Hashimoto’s thyroiditis found that oxidative stress markers — a condition that causes chronic inflammation — were lower in those who ate fruits and vegetables more frequently.
Vegetables, fruits, spices, and fatty fish have powerful anti-inflammatory properties.
Nutrient-dense, whole-food diets
Following a diet low in added sugar and highly processed foods but rich in whole food, nutrient-dense foods may help improve your health, manage your weight, and reduce Hashimoto’s-related symptoms.
Suggested read: No-Carb Diet: Benefits, Downsides, and Foods List
Whenever possible, prepare your meals at home using nutritious foods like vegetables, fruits, proteins, healthy fats, and fiber-rich carbs.
These foods offer powerful antioxidant and anti-inflammatory benefits.
Other diet tips
Some research indicates that certain low-carb diets may help reduce body weight and thyroid antibodies in people with Hashimoto’s thyroiditis.
These diets provide 12–15% of daily calories from carbs and restrict goitrogenic foods. Goitrogens are substances found in cruciferous vegetables and soy products that may interfere with thyroid hormone production.
Yet, cruciferous vegetables are highly nutritious, and cooking them diminishes their goitrogenic activity. Thus, it’s unlikely that they interfere with thyroid function unless eaten in extremely large amounts.
Some evidence suggests that soy harms thyroid function, so many people with Hashimoto’s avoid soy products. Nonetheless, more research is needed.
Summary: Going gluten-free, avoiding dairy, and following a nutrient-dense, anti-inflammatory diet are just a few tips that may improve Hashimoto’s thyroiditis symptoms.
Helpful supplements for Hashimoto’s
Several supplements may help lower inflammation and thyroid antibodies in people with Hashimoto’s thyroiditis. Plus, those with this condition are more likely to be deficient in certain nutrients, so supplementing may be necessary.
Beneficial supplements include:
- Selenium. Studies show that taking 200 mcg of selenium daily may help reduce antithyroid peroxidase (TPO) antibodies and improve well-being in people with Hashimoto’s thyroiditis.
- Zinc. Zinc is essential for thyroid function. Research suggests that taking 30 mg of zinc daily may improve thyroid function in people with hypothyroidism when used alone or alongside selenium.
- Curcumin. Animal and human studies have shown that this powerful anti-inflammatory and antioxidant compound may protect the thyroid. Plus, it may help treat autoimmune diseases in general.
- Vitamin D. People with Hashimoto’s thyroiditis have been shown to have significantly lower levels of this vitamin than the general population. Furthermore, studies link low vitamin D levels with Hashimoto’s thyroiditis severity.
- B complex vitamins. People with Hashimoto’s thyroiditis likewise tend to be low in vitamin B12. A high-quality B complex vitamin boosts B12 and other important B vitamins.
- Magnesium. Low levels of this mineral are associated with an increased risk of Hashimoto’s thyroiditis and higher thyroid antibodies. Plus, correcting magnesium deficiencies may improve symptoms in people with thyroid disease.
- Iron. People with Hashimoto’s thyroiditis are more likely to develop anemia. Iron supplements may be needed to correct a deficiency.
Other supplements like fish oil, alpha-lipoic acid, and N-acetyl cysteine may also help people with Hashimoto’s thyroiditis.
Suggested read: Keto Diet Meal Plan and Menu to Transform Your Body
Supplementing with high doses of iodine without an iodine deficiency may lead to adverse effects in those with Hashimoto’s. Don’t take high-dose iodine supplements unless a healthcare professional has directed you.
Summary: Many vitamin and mineral supplements, including zinc, vitamin D, and magnesium, may benefit those with Hashimoto’s thyroiditis.
Foods to eat
If you have Hashimoto’s thyroiditis, a nutrient-dense diet may help reduce the severity of your symptoms and improve your overall health. Focus on the following foods:
- Fruits: berries, pears, apples, peaches, citrus fruits, pineapple, bananas, etc.
- Non-starchy vegetables: zucchini, artichokes, tomatoes, asparagus, carrots, peppers, broccoli, arugula, mushrooms, etc.
- Starchy vegetables: sweet potatoes, potatoes, peas, acorn and butternut squash, etc.
- Healthy fats: avocados, avocado oil, coconut oil, olive oil, unsweetened coconut flakes, full-fat yogurt, coconut yogurt, etc.
- Animal protein: salmon, eggs, cod, turkey, shrimp, chicken, etc.
- Gluten-free grains: brown rice, rolled oats, quinoa, brown rice pasta, etc.
- Seeds, nuts, and nut butter: cashews, almonds, macadamia nuts, sunflower seeds, pumpkin seeds, natural peanut butter, almond butter, etc.
- Beans and lentils: chickpeas, black beans, lentils, etc.
- Dairy and nondairy substitutes (fortified with calcium and/or vitamin D): coconut milk, coconut yogurt, almond milk, cashew milk, full-fat unsweetened yogurt, goat cheese, etc.
- Spices, herbs, and condiments: turmeric, basil, rosemary, paprika, saffron, black pepper, salsa, tahini, honey, lemon juice, apple cider vinegar, etc.
- Beverages: water, unsweetened tea, sparkling water, etc.
Remember that some people with Hashimoto’s thyroiditis avoid some foods mentioned above, such as grains and dairy. Experimenting with your diet to determine what foods work best for you is important.
Summary: Whole, nutrient-dense foods should make up most of any healthy diet and may be especially helpful if you have Hashimoto’s thyroiditis.
Foods to avoid
Eliminating or restricting the following foods may help reduce Hashimoto’s symptoms and improve your overall health:

- Added sugars and sweets: soda, energy drinks, cakes, ice cream, pastries, cookies, candy, sugary cereals, table sugar, etc.
- Fast food and fried foods: french fries, hot dogs, fried chicken, etc.
- Refined grains: white pasta, white bread, white flour tortillas, bagels, etc.
- Highly processed foods and meats: frozen dinners, margarine, microwave dinners, bacon, sausage, etc.
- Gluten-containing grains and foods: wheat, barley, rye, crackers, bread, etc.
Some healthcare professionals suggest that people with Hashimoto’s thyroiditis also avoid soy and dairy — and sometimes even nightshades and all grains.
However, although these recommendations may help many individuals, it’s important to experiment with your diet to find the best method for you.
Working with a dietitian specializing in autoimmune diseases like Hashimoto’s thyroiditis can help you narrow down potentially problematic foods and set up an eating pattern to help you feel your best.
Summary: Steering clear of added sugar, highly processed foods, and gluten-containing grains may help reduce Hashimoto’s symptoms and improve overall health.
Other lifestyle modifications to try
Getting plenty of sleep, reducing stress, and practicing self-care are extremely important for those with Hashimoto’s thyroiditis.
A study on 60 women with Hashimoto’s disease found that engaging in stress reduction practices helped reduce their depression and anxiety, improve their overall quality of life, and lower thyroid antibodies.
Letting your body rest when you’re feeling fatigued is important as well.
Additionally, it’s best to take thyroid medication on an empty stomach at least 30–60 minutes before breakfast or at least 3–4 hours after dinner for maximum absorption.
Even coffee and dietary supplements interfere with thyroid medication absorption, so it’s best to consume only water for at least 30 minutes after taking your medication.
A healthcare professional can answer any questions about how to ensure maximum absorption.
Keep in mind that when you’re first starting medication, it may take a few weeks or longer to start feeling better. If your symptoms aren’t improving, discuss other options with a healthcare professional.
Suggested read: Low-Sodium Diet: Benefits, Food Lists, Risks, and More
As Hashimoto’s symptoms may significantly affect your quality of life and mental health, be sure to find a healthcare team that you trust. This may take some time, but it’s essential to getting the right treatment.
Summary: Reducing stress, getting plenty of rest, and practicing self-care are essential for those with Hashimoto’s thyroiditis. Finding a healthcare professional whom you trust is also key.
Diagnosis and symptoms
It’s thought that Hashimoto’s thyroiditis develops from an immune defect coupled with environmental factors, though these factors aren’t fully understood.
Diagnosis depends on symptoms and laboratory results.
Lab results indicating Hashimoto’s thyroiditis include elevated thyroid-stimulating hormone (TSH), low levels of free thyroxine (FT4), and increased anti-thyroid peroxidase (anti-TPO) antibodies.
Some people with Hashimoto’s thyroiditis also have elevated TSH receptor-blocking antibodies (TBII) and antithyroglobulin (anti-Tg) antibodies. These antibodies attack the thyroid gland.
The disease’s destruction of the thyroid is intermittent. During its early stages, people may present with symptoms and lab results that indicate hyperthyroidism — or even have normal lab values.
As such, Hashimoto’s thyroiditis is often difficult to detect, and individuals may go for months without the proper diagnosis. Up to one-third of people treated for hypothyroidism don’t receive adequate or proper treatment.
Hashimoto’s thyroiditis affects both women and men, but women are 5–10 times more likely to be diagnosed. Risk increases with age, and most women are diagnosed between 30 and 50.
The peak ages for the general population combined for Hashimoto’s thyroiditis are between 45 and 65.
This condition is usually treated with synthetic or natural thyroid hormones. Synthetic ones include levothyroxine (Synthroid) and liothyronine (Cytomel), while natural ones include Armour Thyroid and Nature Throid.
Symptoms
Because Hashimoto’s thyroiditis affects nearly every organ system in your body, it’s associated with various symptoms. These include:
Suggested read: Vegetarian Keto Diet Plan: Benefits, Risks, Foods & Meal Ideas
- weight gain
- extreme fatigue
- poor concentration
- thinning, coarse hair
- dry skin
- slow or irregular heart rate
- decreased muscle strength
- shortness of breath
- decreased exercise tolerance
- cold intolerance
- elevated blood pressure
- brittle nails
- constipation
- neck pain or thyroid tenderness
- depression and anxiety
- menstrual irregularities
- insomnia
- voice changes
Untreated or improperly treated Hashimoto’s thyroiditis may lead to serious side effects, such as an increased risk of heart disease, cognitive disorders, and even death.
Summary: Hashimoto’s symptoms vary widely, including weight gain, fatigue, cold intolerance, and constipation. The condition is diagnosed based on symptoms and lab results.
Summary
Hashimoto’s thyroiditis is a common autoimmune condition that affects the thyroid. It causes numerous symptoms that may persist even if you take thyroid medication.
Research shows that dietary and lifestyle changes can significantly improve your symptoms and overall health. However, every person with Hashimoto’s thyroiditis is different, so finding a dietary pattern that suits your needs is fundamental.
A dietitian or other healthcare professional who specializes in autoimmune diseases may be able to help you find an eating pattern that works for you.
 Lose weight
Lose weight
 Gain muscles
Gain muscles
 Eat healthy
Eat healthy
 Explore new cuisines
Explore new cuisines
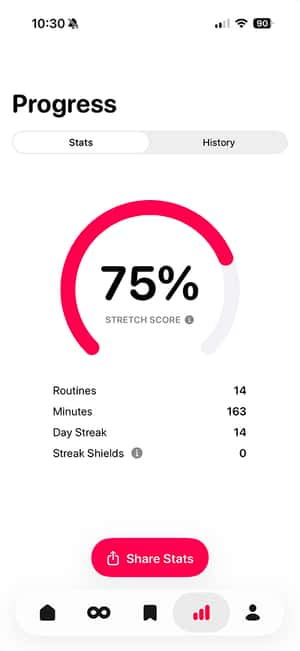
 Available on the App Store
Available on the App Store