Since diabetes is a disease characterized by high blood sugar levels, many people wonder whether eating sugar can cause it.

While it’s true that eating large amounts of added sugar may increase your risk of diabetes, sugar intake is just one piece of the puzzle.
Many other factors — including overall diet, lifestyle, and genetics — also impact your risk.
This article reviews sugar’s role in developing diabetes and provides tips for preventing the disease.
In this article
What is diabetes?
Diabetes occurs when your body is no longer able to effectively regulate blood sugar levels.
This can happen when your pancreas stops producing enough insulin, when your cells become resistant to the insulin that is produced, or both.
Insulin is the hormone required to move sugar out of your bloodstream and into your cells — so both scenarios result in chronically elevated blood sugar levels.
High blood sugar levels over a long period can lead to complications like an increased risk of heart disease, as well as nerve and kidney damage, so it is important to keep them in check.
There are two main types of diabetes, each with different causes:
- Type 1: Occurs when your immune system attacks your pancreas, destroying its ability to produce insulin.
- Type 2: Occurs when your pancreas stops producing enough insulin, when your body’s cells no longer respond to the insulin it produces, or both.
Type 1 diabetes is relatively rare, largely genetic, and only accounts for 5–10% of all diabetes cases.
Type 2 diabetes — which will be the focus of this article — accounts for more than 90% of diabetes cases and is mainly triggered by diet and lifestyle factors.
Summary: Type 2 diabetes is the most common form of diabetes. It occurs when your body stops producing enough insulin or when cells become resistant to the insulin produced, leading to chronically elevated blood sugar levels.
How sugar is metabolized
When most people talk about sugar, they’re referring to sucrose, or table sugar, which is made from sugar beets or sugarcane.
Sucrose is made up of one molecule of glucose and one molecule of fructose bonded together.

When you eat sucrose, the glucose and fructose molecules are separated by enzymes in your small intestine before being absorbed into your bloodstream.
This raises blood sugar levels and signals your pancreas to release insulin. Insulin shuttles glucose out of the bloodstream and into your cells where it can be metabolized for energy.
While a small amount of fructose can also be taken up by cells and used for energy, the majority is carried to your liver where it is converted to either glucose for energy or fat for storage.
If you eat more sugar than your body can use for energy, the excess will be converted into fatty acids and stored as body fat.
Since fructose can be converted to fat, high intakes tend to increase triglyceride levels, which may increase your risk of heart disease and fatty liver.
A high intake of fructose is also associated with higher uric acid levels in the blood. If these uric acid crystals settle in your joints, a painful condition known as gout can develop.
Summary: Glucose from sugar is mostly used by your body for energy, while fructose is taken to your liver for conversion into glucose or fat. High fructose intake has been linked to elevated triglycerides, fatty liver, and gout.
Does sugar increase your risk of diabetes?
A large number of studies have found that people who regularly drink sugar-sweetened beverages have a roughly 25% greater risk of type 2 diabetes.
Suggested read: Refined Sugar: Downsides, Food Sources, and How to Avoid It
Drinking just one sugar-sweetened beverage per day increases your risk by 13%, independent of any weight gain it may cause.
Additionally, countries where sugar consumption is highest also have the highest rates of type 2 diabetes, while those with the lowest consumption have the lowest rates.
The link between sugar intake and diabetes still holds even after controlling for total calorie intake, body weight, alcohol consumption, and exercise.
While these studies do not prove that sugar causes diabetes, the association is strong.
Many researchers believe that sugar increases diabetes risk both directly and indirectly.
It may directly increase risk because of the impact fructose has on your liver, including promoting fatty liver, inflammation, and localized insulin resistance.
These effects may trigger abnormal insulin production in your pancreas and increase your risk of type 2 diabetes.
Eating large amounts of sugar can also indirectly raise diabetes risk by contributing to weight gain and increased body fat — which are separate risk factors for developing diabetes.
What’s more, animal studies suggest that eating a lot of sugar may disrupt the signaling of leptin, a hormone that promotes feelings of fullness, leading to overeating and weight gain.
To reduce the negative effects of high sugar consumption, the WHO recommends getting no more than 10% of your daily calories from added sugars that are not naturally found in foods.
Summary: Added sugars, especially from sugar-sweetened beverages, are strongly linked to the development of type 2 diabetes. This is likely due to sugar’s direct effect on your liver, as well as its indirect effect of increasing body weight.
Natural sugars don’t have the same effect
While eating large amounts of added sugars has been linked to diabetes, the same is not true for natural sugars.
Suggested read: 11 Key Factors That Cause Belly Fat Gain
Natural sugars are sugars that exist in fruits and vegetables and have not been added during manufacturing or processing.
Since these types of sugar exist in a matrix of fiber, water, antioxidants, and other nutrients, they’re digested and absorbed more slowly and less likely to cause blood sugar spikes.
Fruits and vegetables also tend to contain far less sugar by weight than many processed foods, so it is easier to keep your consumption in check.
For example, a peach has approximately 8% sugar by weight, while a Snickers bar contains 50% sugar by weight.
While research is mixed, some studies have found that eating at least one serving of fruit per day reduces diabetes risk by 7–13% compared to eating no fruit.
What about fruit juice?
Research is mixed on whether drinking 100% fruit juice increases diabetes risk.
Several studies have found a link between drinking fruit juice and developing diabetes, perhaps due to juice’s high sugar and low fiber contents.
However, not all studies have replicated these results, so more research is needed.
What about natural sweeteners?
Though some natural sweeteners, like honey and maple syrup, are generally not as heavily processed as table sugar or corn syrup, they are still relatively pure sources of sugar and contain almost no fiber.
Many other sweeteners, marketed as being “natural,” should also be considered added sugar. These include agave syrup, coconut sugar, and cane sugar, to name a few.
Therefore, they should be consumed in moderation like all added sugars, ideally making up less than 10% of your daily calories.
Summary: While added sugars are strongly linked to the development of diabetes, natural sugars found in whole fruits and vegetables don’t have the same effect.
Do artificial sweeteners increase diabetes risk?
Artificial sweeteners are man-made, sweet-tasting substances that cannot be metabolized by humans for energy. As such, they provide sweetness without any calories.
Though artificial sweeteners don’t spike blood sugar levels, they have still been linked to the development of insulin resistance and type 2 diabetes.
Drinking just one can of diet soda per day has been associated with a 25–67% increased risk of type 2 diabetes, compared to drinking no diet soda at all.
It’s unclear why artificial sweeteners increase diabetes risk, but there are a variety of theories.
One thought is that artificially sweetened products increase cravings for sweet-tasting foods, leading to higher sugar consumption and weight gain, which increases diabetes risk.
Suggested read: How Much Sugar Should You Eat Per Day? Safe Daily Intake Guide
Another idea is that artificial sweeteners disrupt your body’s ability to properly compensate for calories consumed from sugar since your brain associates the sweet taste with zero calories.
Some research has found that artificial sweeteners can change the type and number of bacteria that live in your colon, which may contribute to glucose intolerance, weight gain, and diabetes.
While there does appear to be a link between artificial sweeteners and diabetes, more research is needed to understand exactly how they’re related.
Summary: While artificially sweetened foods and beverages contain no sugar and fewer calories than sugar-sweetened alternatives, they’re still linked to the development of diabetes. More research is needed to understand why.
Other risk factors for diabetes
While consuming large amounts of added sugar is linked to an increased risk of diabetes, many other factors are at play, such as:
- Bodyweight: Research shows that obesity is one of the main risk factors for type 2 diabetes but that losing just 5–10% body weight can reduce the risk.
- Exercise: People who live sedentary lifestyles have nearly twice the risk of developing type 2 diabetes compared to those who are active. Just 150 minutes per week of moderate activity can reduce the risk.
- Smoking: Smoking 20 or more cigarettes per day more than doubles your risk of diabetes, but quitting brings the risk nearly back to normal.
- Sleep apnea: Sleep apnea, a condition in which breathing is obstructed during the night, is a unique risk factor for diabetes.
- Genetics: The risk of developing type 2 diabetes is 40% if one of your parents has it and nearly 70% if both parents have it — suggesting a genetic link.
Summary: While sugar intake can influence diabetes risk, it’s far from the only contributing factor. Diet, lifestyle, and genetic factors also play a role.
How to eat to lower your risk of diabetes
In addition to cutting back on added sugars, there are many other dietary changes you can make to reduce your diabetes risk:

- Follow a whole-food diet: Diets rich in nuts, fruits, vegetables, and whole grains have been linked to a reduced risk of diabetes.
- Drink coffee: Drinking coffee may reduce your risk of type 2 diabetes. Each daily cup is associated with a 7% lower risk of diabetes.
- Eat green leafy vegetables: Eating a diet rich in green leafy vegetables has been linked to a 14% lower risk of diabetes.
- Limit alcohol consumption: Moderate alcohol consumption — defined as about 0.5–3.5 drinks per day — has been linked to a roughly 30% lower risk of diabetes, compared to completely abstaining or drinking heavily.
If reducing your intake of added sugars feels overwhelming, you can start by simply reducing your intake of sugar-sweetened beverages, which are the primary source of added sugars in the standard American diet.
This one small change could make a big impact.
Carefully reading nutrition labels is another must, since there are over 50 different names for sugar used in food products. Learning to notice them is the first step in reducing your consumption.
Thankfully, there are many ways to cut back on sugar while still enjoying a flavorful and nutrient-dense diet, so you don’t have to feel deprived.
Summary: Eating fewer added sugars can reduce your risk of diabetes, as can a diet rich in fruits, vegetables, and coffee with moderate alcohol consumption.
Summary
Excessive amounts of added sugars have been associated with an increased risk of type 2 diabetes, likely due to negative effects on the liver and a higher risk of obesity.
Natural sugars like those found in fruits and vegetables are not linked to diabetes risk — whereas artificial sweeteners are.
In addition to sugar consumption, overall diet quality, body weight, sleep quality, exercise, and genetics all play a role in the development of this disease.
Eating a diet rich in fruits, vegetables, nuts, and coffee, consuming alcohol in moderation, maintaining a healthy body weight, and exercising regularly can help reduce your risk of type 2 diabetes.
Suggested read: 6 Reasons Why High-Fructose Corn Syrup Is Bad for You
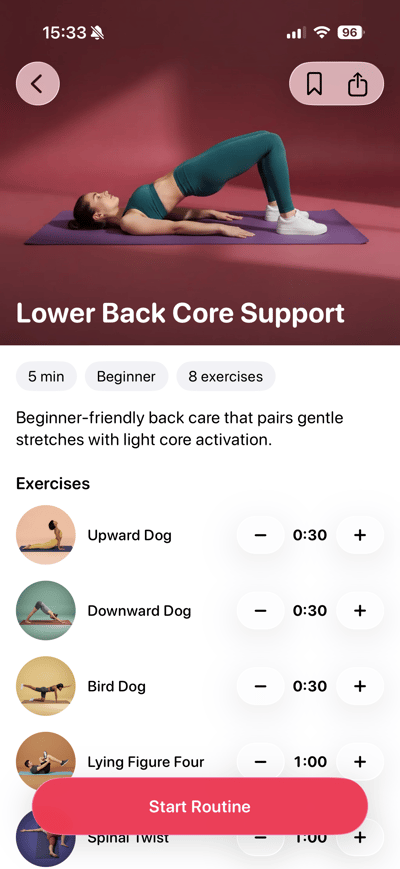
 Lose weight
Lose weight
 Gain muscles
Gain muscles
 Eat healthy
Eat healthy
 Explore new cuisines
Explore new cuisines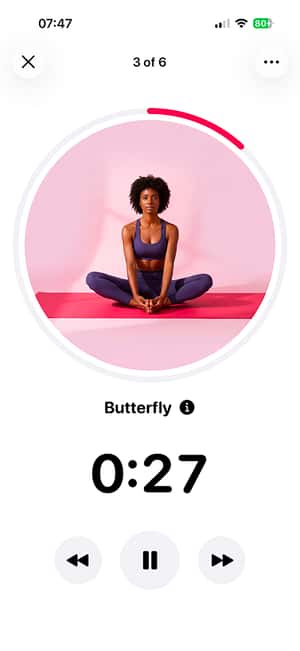
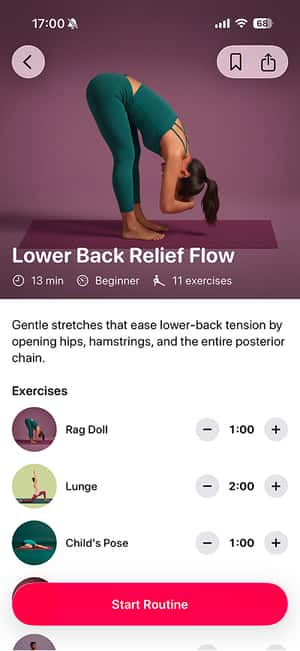
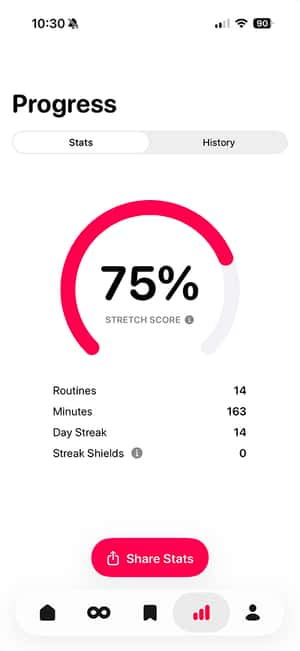
 Available on the App Store
Available on the App Store