Doctors frequently utilize BMI to monitor health. However, for many, it is not a precise gauge of obesity, and its accuracy varies among individuals.

Researchers commonly employ Body Mass Index (BMI) to observe obesity trends across populations.
It’s also a tool healthcare professionals use to evaluate an individual’s health.
Yet, there has been growing concern in the medical field about using BMI as a health and obesity metric due to its notable shortcomings, especially when evaluating the health of Black, Hispanic, and other groups.
Despite these concerns, some health institutions still advocate maintaining a specific BMI to decrease disease risk.
This article delves into the concept of BMI and its relevance to women’s health.
In this article
BMI chart and calculator
BMI does not distinguish between men and women. It’s a simple formula that uses height and weight to calculate a number representing a person’s body fat levels.
These numbers fit within the following categories:
- Less than 16.5: severe underweight
- Less than 18.5: underweight
- 18.5–24.9: normal weight
- 25.0–29.9: overweight
- 30.0–34.9: obesity class 1
- 35.0–39.9: obesity class 2
- 40 or greater: obesity class 3
This calculator can help you determine your BMI and your estimated daily calories, although it is not specifically for women:
BMI Calculator
Enter your details in the calculator below to determine your BMI.
Does the same chart suit all women?
While a chart can be helpful, BMI is not a one-size-fits-all concept. Depending on a person’s ethnicity, muscularity, and other factors, doctors may recommend different cutoff points.
White, Black, and Hispanic women
BMI does not inherently distinguish between people of different genetic backgrounds. However, as this article will discuss later, different BMI cutoffs have been developed for Asian and South Asian populations.

White, Black, and Hispanic women are considered to be at a “healthy weight” when their BMI lies between 18.5 and 24.9.
For example, according to the Centers for Disease Control and Prevention (CDC), a woman 65 inches (1.65 meters) tall would fall within a normal BMI range if she weighed 111–150 pounds (50–68 kg).
However, women differ in body shape and body composition.
For example, research shows that Mexican American women tend to have a different body fat distribution than white or Black women. Additionally, Black women tend to have more muscle mass than white or Mexican American women.
On average, Mexican American women have more body mass in their abdomen. One review found that Mexican American women may have 3–5% more body fat and a larger waist circumference than white or Black women with similar BMIs.
These differences between women of various ethnicities are based on data averaged over many people.
However, a person’s ethnicity does not determine their weight, body fat distribution, proportion of muscle mass, waist circumference, or other body metrics. Every person is different.
This means that even if two women have the same BMI, they can have very different regional body fat distribution and muscle mass.
Furthermore, researchers acknowledge that the link between BMI and mortality risk is much weaker among Black women than among white women.
This is because BMI is a weaker indicator of body fat levels in Black women and because, on average, Black women have different fat distribution than white women. BMI is not associated with blood fat levels in Black women as in white women.
Suggested read: Weight Loss vs. Fat Loss: How to Tell the Difference
Studies have shown that healthcare professionals are more likely to misclassify Black women as having obesity because of their higher muscle mass percentage.
Asian and South Asian women
Research shows that Asian and South Asian populations have more body fat relative to their body weight than white populations. Health conditions like type 2 diabetes occur at lower BMI levels in Asian populations than in white populations.
This has led to changes in BMI cutoffs for Asian populations.
Asian and South Asian women are overweight when their BMI is 23–27.5 and are considered to have obesity when their BMI is over 27.5.
However, several different BMI cutoffs for Asian populations have been suggested.
Bodybuilders and athletes
The BMI system often misclassifies women with significant amounts of muscle mass as overweight or obese, even though their body fat levels are low. This includes people such as bodybuilders and professional athletes.
This is because BMI doesn’t differentiate between muscle mass and fat mass, which is why people shouldn’t use BMI to measure body composition.
Postmenopausal women
Older women tend to have lower muscle mass and more fat located in their midsection than younger women.
This is due to age-related changes in hormone levels, slowing of physical activity, and changes in torso length due to osteoporosis.
Even though an older woman may have the same BMI as a younger woman, the older woman will likely have less muscle mass and more body fat, which increases her risk of disease.
A 2016 study that included 1,329 postmenopausal women found that the BMI cutoff of 30 was not an accurate indicator of obesity in this population. The researchers pointed out that BMI may not indicate obesity in many postmenopausal women who do have obesity.
Weight gain recommendations during pregnancy based on BMI
Healthcare professionals recommend that women gain a certain amount of weight during pregnancy based on their prepregnancy BMI range.
Suggested read: Malnutrition: Definition, Symptoms, Causes & Treatment
Here are the Institute of Medicine guidelines for weight gain during pregnancy:
Underweight (under 18.5)
- Total recommended weight gain: 28–40 pounds (12.5–18 kg)
- Mean rate of weight gain in the second and third trimesters: 1 pound (0.51 kg) per week
Normal weight (18.5–24.9)
- Total recommended weight gain: 25–35 pounds (11.5–16 kg)
- Mean rate of weight gain in the second and third trimesters: 1 pound (0.42 kg) per week
Overweight (25.0–29.9)
- Total recommended weight gain: 15–25 pounds (7–11.5 kg)
- Mean rate of weight gain in the second and third trimesters: 0.6 pounds (0.28 kg) per week
Obesity (30 or greater)
- Total recommended weight gain: 11–20 pounds (5–9 kg)
- Mean rate of weight gain in the second and third trimesters: 0.5 pounds (0.22 kg) per week
Even though you can use these recommendations as helpful guidelines, working with your healthcare provider is essential. They can help you determine a healthy weight gain during pregnancy based on your specific needs and overall health.
Remember that weight gain guidelines differ for women carrying more than one baby.
Summary: A “normal” BMI for women ranges from 18.5–24.9. However, BMI is not an accurate measure of obesity in many people. It tends not to be a good indicator in postmenopausal women, athletes, and Black and Hispanic women.
Is BMI a good indicator of health?
Adolphe Quetelet, a Belgian astronomer and statistician, developed BMI 180 years ago. However, BMI didn’t gain much popularity among researchers until epidemiologist Ancel Keys identified it as an effective way to track body fat proportions at a population level.
BMI uses a person’s height and weight to estimate their body fat.
Issues with BMI
Using BMI as a marker of health is problematic for several reasons.
Even though some health professionals use BMI to categorize individuals based on body fat, it doesn’t actually take body fat or lean body mass into account. This means BMI doesn’t recognize the difference between muscle and fat.
Suggested read: Body recomposition: Lose fat and gain muscle at the same time
For this reason, BMI might categorize someone with a very high percentage of muscle mass as having excess weight or obesity, even if they have low body fat levels.
Another shortcoming of BMI is that it doesn’t indicate where fat is stored in the body. Therefore, it doesn’t account for variation in fat distribution between sexes or different body types. It also doesn’t consider age-related decline in muscle mass.
The system may classify a small-framed person in a healthy BMI range, even if they have significant belly fat. However, this person may actually be at risk because belly fat is significantly linked to many chronic diseases and early death.
In other words, a person with a “healthy” BMI may actually be at significant risk of disease, surgical complications, and increased mortality.
Additionally, health is multidimensional. There are many factors a person should consider when assessing their overall health and risk of disease.
Experts argue that BMI is much too simplistic a measure to use as an indicator of health.
Summary: BMI doesn’t consider body fat or lean body mass. It also doesn’t consider where fat is stored in the body. Because of these issues, it may provide misleading health information for some people.
Benefits of BMI
Despite its significant shortcomings, BMI is one of the most effective, easiest, and cheapest options for researchers to track obesity at the population level, which is extremely important for medical research.
Additionally, a high BMI correlates with higher body fat levels, and studies have shown that BMI can accurately determine disease and mortality risk in individuals.
People whose BMI classifies them as having obesity are at a significantly greater risk of early death and developing chronic diseases, including heart disease and kidney disease, than people within the “normal” BMI range.

People whose BMI classifies them as underweight are also more at risk of early death and developing disease.
Plus, even though people should not view BMI as a reliable measure of health on its own, healthcare professionals can use BMI in combination with other diagnostic tools to assess a person’s health and monitor their risk of disease.
Other tools include waist circumference and laboratory values such as cholesterol levels.
Other ways to measure health
There are other, more appropriate ways to measure health than BMI.
Here are a few more accurate ways to measure body composition:
- DEXA. Dual-energy X-ray absorptiometry (DEXA) is an accurate way to measure total body fat, muscle mass, and bone mass. Talk to your healthcare provider if you’re interested in a DEXA scan.
- Body circumference measurements. Waist circumference is an important indicator of disease risk. On average, a circumference over 35 inches (89 cm) in women, or over 31 inches (79 cm) in Asian women, is associated with increased disease risk.
- Skinfold calipers. Skinfold calipers are another relatively easy way to measure body fat. However, they can be uncomfortable and require training before taking accurate measurements.
Many other ways to measure body composition include bioimpedance spectroscopy (BIS) and air displacement plethysmography. However, these are typically available only in medical settings or in certain fitness centers.
Even though these methods can measure body composition, there are many other factors to consider regarding overall health and well-being.
For example, getting your blood tested is extremely important when assessing your health and risk of disease.
For this reason, women should regularly see a healthcare professional, who can recommend blood work, such as cholesterol testing, based on individual background and health status.
When assessing your physical and mental health, a healthcare professional should also consider your dietary patterns, activity levels, genetics, sleep habits, mental health, stress, and socioeconomic status.
Suggested read: Types of Belly Fat: What They Are and How to Lose Belly Fat
Summary: Accurate body composition measures include DEXA and body circumference measurements. There are several ways to measure health, many of which have nothing to do with body weight or body composition.
Summary
While healthcare experts recognize the limitations of BMI, it still serves as a valuable metric for gauging public health on a broad scale.
For individuals, BMI can be a rough gauge of health, but it might not be precise for everyone.
A BMI between 18.5–24.9 is generally considered healthy for most women.
Although BMI can be useful for initial screenings in the medical field, it shouldn’t be the sole criterion to judge someone’s overall body fat or health.
Remember, health encompasses more than just weight or body composition. A comprehensive health evaluation should consider factors like blood tests, dietary habits, physical activity, and sleep patterns.
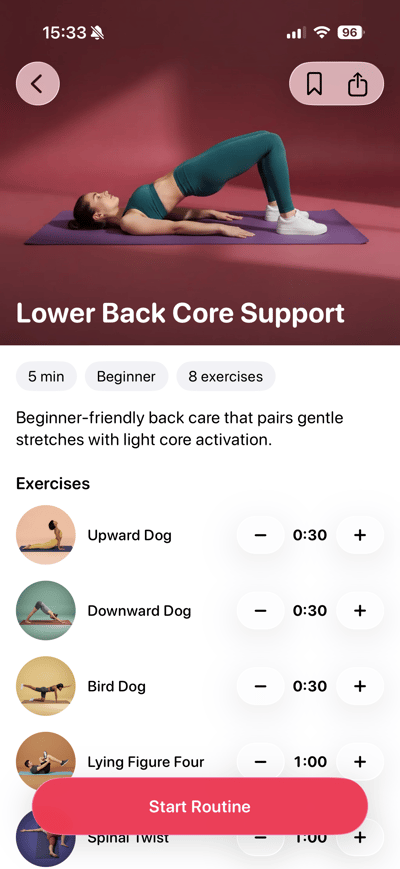
 Lose weight
Lose weight
 Gain muscles
Gain muscles
 Eat healthy
Eat healthy
 Explore new cuisines
Explore new cuisines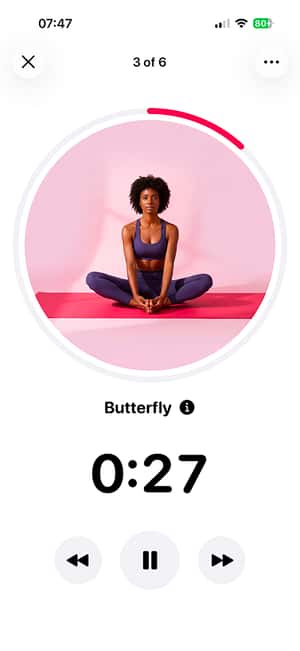
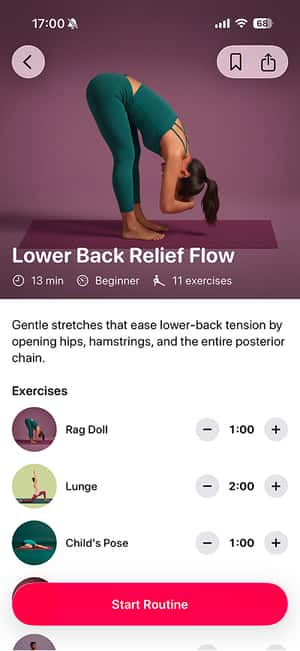
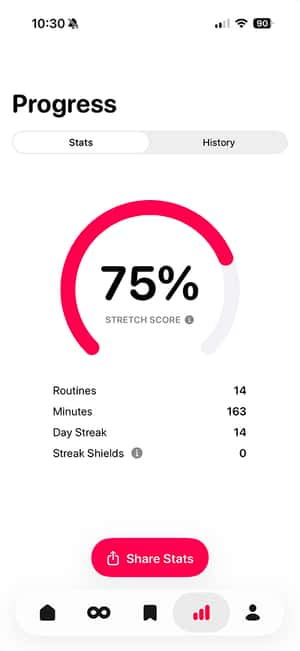
 Available on the App Store
Available on the App Store